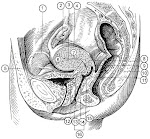
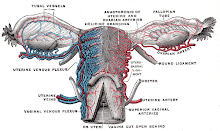
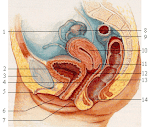
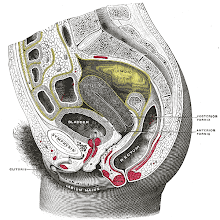
The Pelvis The pelvis is the inferior part of the trunk
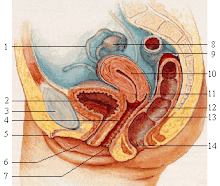
and the pelvic cavity is the basin-shaped inferior part of the abdominopelvic cavity, which is located inferior to the plane of the pelvic brim. The pelvic cavity is bounded inferiorly by
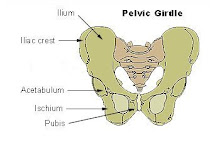
the pelvic diaphragm. This forms the pelvic floor and separates the pelvis from the perineum. The circumference of the superior pelvic aperture (pelvic inlet) is outlined on each side by the pelvic brim and extends from the superior border of the pubic symphysis anteriorly to the promontory of the sacrum posteriorly. The Bony Pelvis This is the skeleton of the pelvis. It surrounds the pelvic cavity and forms
the pelvic girdle for the attachment of the lower limbs. It is formed anteriorly and laterally by the two hip bones and posteriorly by the sacrum and coccyx. Anteriorly, the two pubic bones meet at the pubic symphysis . The skeleton of the pelvis was covered in
Medicine 1 (ANAT1006). The Pelvic Brim The pelvic cavity is located inferior to the plane of the pelvic brim. This is an oblique plane that forms an angle of about 55 degrees to the horizontal. It coincides with a line joining the sacral promontory to the superior border of the pubic symphysis . This line also gives the anteroposterior (AP) diameter of the superior pelvic
aperture of pelvic inlet. The pelvic brim is formed from the
following structures: 1. Superior margin of the pubic symphysis ; 2. The pubic crest; 3. The pecten pubis (pectineal line of the pubis); 4. The arcuate line of the ilium; 5. The anterior border of the ala of the sacrum; 6. And the promontory of the sacrum. The pelvis is divided into a pelvis major (false pelvis), which is part of the abdominal cavity, and a pelvis minor (true or "obstetric" pelvis), which
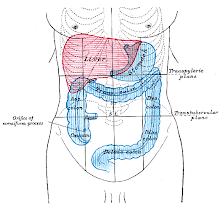
contains the pelvic cavity. Back to top The Pelvis Major The false pelvis lies superior to the superior pelvic aperture (pelvic inlet) or pelvic brim. Its cavity is part of the abdominal cavity and it contains abdominal viscera. The pelvis major is bounded anteriorly by
the abdominal wall, laterally by the iliac fossae, and posteriorly by L5 and S1 vertebrae. The Pelvis Minor The true pelvis lies inferior to the pelvic inlet and pelvic brim. It is limited inferiorly by the inferior pelvic aperture (pelvic outlet). This is closed by the pelvic diaphragm that is composed mainly of the levator ani muscles. Its inferior boundary corresponds roughly
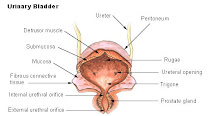
to a line joining the tip of the coccyx to the inferior border of the pubic symphysis . The cavity of the pelvis minor is the pelvic cavity and it contains pelvic viscera (e.g., the urinary bladder). It is tilted anteroinferiorly when it is in the anatomical position. The Walls of the Pelvis Minor The posterior wall, which is notably longer than its anterior wall, is formed by
the concave pelvic surface of the sacrum and coccyx. The anterior wall is formed by the pubic symphysis , the body of the pubis, and the pubic rami. The lateral walls are formed by the pelvic aspects of the ilium and ischium. Back to top The Superior Pelvic Aperture (Pelvic
Inlet) The pelvic inlet is variable in contour. Sexual, racial and nutritional differences
influence its shape. It is heart-shaped in males and some females. In most females, this opening is larger than in the male and is rounded or oval in contour. The pelvic inlet is encroached by the sacral promontory. The periphery of the pelvic inlet, formed
by the pelvic brim, is indicated by the linea terminalis (iliopectineal line). This terminal line is an oblique ridge on the internal surface of the ilium, which is continued on the pubis. It forms the inferior boundary of the iliac fossae and separates the true and false pelves. The Inferior Pelvic Aperture (Pelvic
Outlet) The pelvic outlet is bounded: 1. Posteriorly by the sacrum and coccyx; 2. Anteriorly by the pubic symphysis ; 3. And laterally by the ischial tuberosities. It is because of this that it does not have a smooth contour. The plane of this aperture makes an
angle of 10-15 degrees with the horizontal when the pelvis is in the anatomical position. The greater and lesser sciatic notches between the sacrum, coccyx and the
ischial tuberosities are divided into the
respective foramina by the sacrotuberous and sacrospinous ligaments These ligaments give the pelvic outlet a diamond-shape. The subpubic angle is narrow in males and wide in females. Types of Pelves in Caucasian Females 1. Gynaecoid, round with enlarged transverse diameter (41.4%) 2. Android, heart-shaped (32.5%) 3. Anthropoid, long AP diameter (23.5%) 4. Platypelloid, long transverse diameter (2.6%) Main Differences Between the Male and
Female Pelves Feature Male Female General
structure Thick and heavy Thin and light Muscle
attachments Well marked Poorly marked Pelvis major Deep Shallow Pelvis minor Narrow and deep Wide and shallow Superior pelvic
aperture Heart shaped Oval or rounded Inferior pelvic
aperture Comparatively small Comparatively large Subpubic angle Narrow Wide Obturator
foramen Round Oval Acetabulum Large Small Back to top The Vertebropelvic Ligaments The parts of the bony pelvis are bound
together by dense and strong ligaments. The Iliolumbar Ligament This is a strong triangular ligament that
connects the tip of the transverse process of L5 (and occasionally L4) to the iliac crest posteriorly. The inferior fibres of the ligament are
attached to the lateral part of the sacrum; this part called the lateral lumbosacral ligament. These ligaments are important because
they: 1. Limit rotation of L5 vertebra on the sacrum; 2. And assist the vertebral articular
processes in preventing the anterior gliding of L5 on the sacrum. The Sacrotuberous Ligament This passes from the sacrum to the ischial tuberosity. It has a wide attachment to the dorsal surfaces of the sacrum and coccyx and the PSIS. The fibres run inferolaterally, to the superior medial impression on the ischial tuberosity and then extend along its medial margin. The Sacrospinous Ligament This is a thin triangular ligament that
extends from the lateral margin of the sacrum and coccyx to the ischial spine. It is related anteriorly to the coccygeus muscle. The Sacroiliac Ligaments There were covered in Medicine 1
(ANAT1006). Click here to go to the sacroiliac ligaments. Back to top Joints of the Pelvis The Lumbosacral Joints L5 and S1 vertebrae articulate with each other at an anterior intervertebral joint formed by the intervertebral disc between their bodies, and at 2 posterior synovial joints between their articular processes. The L5/S1 intervertebral disc is wedge- shaped because it is thicker anteriorly. The zygapophyseal (facet) joints are synovial joints between the articular processes (inferior ones of L5 and superior ones of S1) of the two
vertebrae. The S1 facets face posteriorly and medially, thereby preventing L5 vertebrae from sliding anteriorly. L5 vertebra is also attached to the ilium
and sacrum by the strong iliolumbar ligaments. The Sacrococcygeal Joint This joint is a secondary cartilaginous joint in which fibrocartilage and ligaments join the articulating bones, the apex of the sacrum and the base of the coccyx. They are united by a thin, fibrocartilaginous intervertebral disc. The sacrococcygeal ligaments correspond to the anterior and posterior longitudinal ligaments or the other intervertebral joints. The sacral and coccygeal cornua (L. horns)
are also united by intercornual ligaments. Until middle age, there is slight
movement of the coccyx during
defecation, and considerable movement
during childbirth. In elderly persons the sacrococcygeal
joint usually becomes ossified and is
obliterated. The Sacroiliac Joints This was covered in Medicine 1
(ANAT1006). Click here to go to the sacroiliac joints. The Pubic Symphysis This was covered in Medicine 1
(ANAT1006). Click here to go to the pubic symphysis. Back to top Walls of the Pelvis The Anterior Pelvic Wall This is formed on each side by (1) the bodies of the pubic bones, and its superior and inferior rami, and (2) the obturator internus muscle and its fascia. The pubic symphysis also forms an important part of the anterior pelvic wall. The Lateral Pelvic Walls The obturator internus muscle cover most of these walls. Their superior parts, near the pelvic brim, are covered by pelvic fascia. Medial to the obturator internus on each side are the obturator nerve and vessels and other branches of the internal iliac artery. The obturator internus passes from the pelvis through the lesser sciatic foramen, and its fibres converge to form a tendon that is attached to the greater trochanter of the femur. The Posterior Pelvic Walls This wall is formed by the sacrum, adjacent parts of the ilium, and the sacroiliac joints and their ligaments. The piriformis muscles line the posterior wall laterally. These pear-shaped muscles (L. pirum, pear + forma, form) occupy a key position
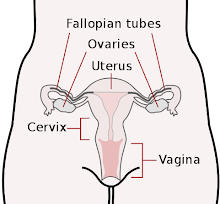
in the gluteal region (buttock). Each piriformis muscle leaves the pelvis minor through the greater sciatic foramen. Medial to the piriformis muscles are the sacral plexus and the internal iliac vessels and their subsidiaries. Back to top The Floor of the Pelvis This is formed mainly by the funnel- shaped pelvic diaphragm, which is composed of the two levator ani and the two coccygeus muscles. This diaphragm closes the inferior pelvic aperture (pelvic outlet), except for a gap in the pelvic floor between the anterior edges of the levator ani muscles. This gap is filled with loose fascia around the prostate (or vagina) and is closed by the urogenital diaphragm and its superior fascia. The pelvic diaphragm also separates the pelvic cavity from the perineum. The musculofascial pelvic diaphragm supports the abdominopelvic viscera. It is slung somewhat like a funnel- shaped hammock between the pubis anteriorly and the coccyx posteriorly. Laterally, it is attached to a thickening of the obturator fascia known as the tendinous arch. The rectum and urethra, and the vagina in women, penetrate the pelvic
diaphragm to reach the exterior. The Levator Ani Muscles These are the largest and most important muscles in the pelvic floor. Posterior to them are the coccygeus muscles, which form the smaller part of the floor. The thin, broad levator ani muscles unite
with its partner to form a hammock-like
sheet of muscle between the pubis
anteriorly and the coccyx posteriorly, and
from one lateral pelvic wall to the other. The levator ani muscles form most of the
floor of the pelvic cavity, which
separates it from the wedge-shaped spaces known as the ischioanal (ischiorectal) fossae. The levator ani muscle is divided into 3 principal parts: the puborectalis, pubococcygeus, and iliococcygeus. The Puborectalis Muscle This arises from the pubis and passes posteriorly, where it unites with its partner to from a U-shaped muscular sling around the anorectal junction. This sling maintains the anorectal flexure. Some fibres of the puborectalis sweep
around the prostate in males and the middle of the vagina in females and are inserted into the central perineal ligament or tendon, or perineal body. This is a fibromuscular mass anterior to the anus. These muscle fibres constitute the levator prostatae and pubovaginalis respectively. The Pubococcygeus Muscle This is the main part of the levator ani. It arises from the pubis and runs posteromedially to insert into the coccyx and anococcygeal ligament. The anococcygeal ligament is the median fibrous intersection of the pubococcygeus muscles. It is located between the anal canal and the tip of the coccyx. The pubococcygeus muscle, as it courses inferiorly and medially, encircles the urethra, vagina, and anus and merges into the perineal body. The Iliococcygeus Muscle This is the thin part of the levator ani. It arises on each side from the tendinous arch of the obturator fascia and the ischial spine. Each muscle passes medially and posteriorly and attaches to the coccyx and anococcygeal ligament. Innervation of the Levator Ani Muscles They are innervated by the perineal branches of the 3rd and 4th sacral nerves, which enter its pelvic surface. Actions of the Levator Ani Muscles As the pelvic diaphragm it resists the downward thrust associated with an increase of intra-abdominal pressure (e.g., coughing). Acting together, the levator ani muscles raise the pelvic floor, thereby assisting the anterior abdominal muscles in compressing the abdominal and pelvic
contents. This action is important part of forced
expiration, coughing, vomiting,
micturition, and fixation of the trunk
during strong movements of the upper
limbs. The parts of the levator ani muscles that
insert into the perineal body (tendinous centre of the perineum) support the prostate (levator prostatae) in males. In females, these parts support the
posterior wall of the vagina
(pubovaginalis). The parts of the levator ani muscles that
insert into the wall of the anal canal holds the anorectal junction anteriorly, thereby increasing the angle between the rectum and anal canal. This prevents the passage of faeces
between the rectum and anal canal when defecation is not desired or is
inconvenient. When these parts contract, they raise the canal over a descending mass of faeces, thereby aiding defecation. During parturition, the levator ani muscles support the foetal head, while the cervix of the uterus is dilating. Back to top The Coccygeus Muscles This is a triangular sheet of muscle that lies against the posterior part of the iliococcygeus muscle with which it is continuous. These along with the levator ani muscle form the pelvic diaphragm. The coccygei form the posterior and smaller part of the pelvic floor, which is formed by the pelvic diaphragm. Lateral attachment: pelvic surfaces of ischial spine and sacrospinous ligament. Medial attachment: lateral margin of the coccyx and S5 vertebra. Innervation: branches of S4 and S5 nerves. The coccygeus muscles assist the levator ani muscles in supporting pelvic viscera. They also support the coccyx and pull it anteriorly, elevating the pelvic floor. The Pelvis The pelvis is the inferior part of the trunk
and the pelvic cavity is the basin-shaped inferior part of the abdominopelvic cavity, which is located inferior to the plane of the pelvic brim. The pelvic cavity is bounded inferiorly by
the pelvic diaphragm. This forms the pelvic floor and separates the pelvis from the perineum. The circumference of the superior pelvic aperture (pelvic inlet) is outlined on each side by the pelvic brim and extends from the superior border of the pubic symphysis anteriorly to the promontory of the sacrum posteriorly. The Bony Pelvis This is the skeleton of the pelvis. It surrounds the pelvic cavity and forms
the pelvic girdle for the attachment of the lower limbs. It is formed anteriorly and laterally by the two hip bones and posteriorly by the sacrum and coccyx. Anteriorly, the two pubic bones meet at the pubic symphysis . The skeleton of the pelvis was covered in
Medicine 1 (ANAT1006). The Pelvic Brim The pelvic cavity is located inferior to the plane of the pelvic brim. This is an oblique plane that forms an angle of about 55 degrees to the horizontal. It coincides with a line joining the sacral promontory to the superior border of the pubic symphysis . This line also gives the anteroposterior (AP) diameter of the superior pelvic
aperture of pelvic inlet. The pelvic brim is formed from the
following structures: 1. Superior margin of the pubic symphysis ; 2. The pubic crest; 3. The pecten pubis (pectineal line of the pubis); 4. The arcuate line of the ilium; 5. The anterior border of the ala of the sacrum; 6. And the promontory of the sacrum. The pelvis is divided into a pelvis major (false pelvis), which is part of the abdominal cavity, and a pelvis minor (true or "obstetric" pelvis), which
contains the pelvic cavity. Back to top The Pelvis Major The false pelvis lies superior to the superior pelvic aperture (pelvic inlet) or pelvic brim. Its cavity is part of the abdominal cavity and it contains abdominal viscera. The pelvis major is bounded anteriorly by
the abdominal wall, laterally by the iliac fossae, and posteriorly by L5 and S1 vertebrae. The Pelvis Minor The true pelvis lies inferior to the pelvic inlet and pelvic brim. It is limited inferiorly by the inferior pelvic aperture (pelvic outlet). This is closed by the pelvic diaphragm that is composed mainly of the levator ani muscles. Its inferior boundary corresponds roughly
to a line joining the tip of the coccyx to the inferior border of the pubic symphysis . The cavity of the pelvis minor is the pelvic cavity and it contains pelvic viscera (e.g., the urinary bladder). It is tilted anteroinferiorly when it is in the anatomical position. The Walls of the Pelvis Minor The posterior wall, which is notably longer than its anterior wall, is formed by
the concave pelvic surface of the sacrum and coccyx. The anterior wall is formed by the pubic symphysis , the body of the pubis, and the pubic rami. The lateral walls are formed by the pelvic aspects of the ilium and ischium. Back to top The Superior Pelvic Aperture (Pelvic
Inlet) The pelvic inlet is variable in contour. Sexual, racial and nutritional differences
influence its shape. It is heart-shaped in males and some females. In most females, this opening is larger than in the male and is rounded or oval in contour. The pelvic inlet is encroached by the sacral promontory. The periphery of the pelvic inlet, formed
by the pelvic brim, is indicated by the linea terminalis (iliopectineal line). This terminal line is an oblique ridge on the internal surface of the ilium, which is continued on the pubis. It forms the inferior boundary of the iliac fossae and separates the true and false pelves. The Inferior Pelvic Aperture (Pelvic
Outlet) The pelvic outlet is bounded: 1. Posteriorly by the sacrum and coccyx; 2. Anteriorly by the pubic symphysis ; 3. And laterally by the ischial tuberosities. It is because of this that it does not have a smooth contour. The plane of this aperture makes an
angle of 10-15 degrees with the horizontal when the pelvis is in the anatomical position. The greater and lesser sciatic notches between the sacrum, coccyx and the
ischial tuberosities are divided into the
respective foramina by the sacrotuberous and sacrospinous ligaments These ligaments give the pelvic outlet a diamond-shape. The subpubic angle is narrow in males and wide in females. Types of Pelves in Caucasian Females 1. Gynaecoid, round with enlarged transverse diameter (41.4%) 2. Android, heart-shaped (32.5%) 3. Anthropoid, long AP diameter (23.5%) 4. Platypelloid, long transverse diameter (2.6%) Main Differences Between the Male and
Female Pelves Feature Male Female General
structure Thick and heavy Thin and light Muscle
attachments Well marked Poorly marked Pelvis major Deep Shallow Pelvis minor Narrow and deep Wide and shallow Superior pelvic
aperture Heart shaped Oval or rounded Inferior pelvic
aperture Comparatively small Comparatively large Subpubic angle Narrow Wide Obturator
foramen Round Oval Acetabulum Large Small Back to top The Vertebropelvic Ligaments The parts of the bony pelvis are bound
together by dense and strong ligaments. The Iliolumbar Ligament This is a strong triangular ligament that
connects the tip of the transverse process of L5 (and occasionally L4) to the iliac crest posteriorly. The inferior fibres of the ligament are
attached to the lateral part of the sacrum; this part called the lateral lumbosacral ligament. These ligaments are important because
they: 1. Limit rotation of L5 vertebra on the sacrum; 2. And assist the vertebral articular
processes in preventing the anterior gliding of L5 on the sacrum. The Sacrotuberous Ligament This passes from the sacrum to the ischial tuberosity. It has a wide attachment to the dorsal surfaces of the sacrum and coccyx and the PSIS. The fibres run inferolaterally, to the superior medial impression on the ischial tuberosity and then extend along its medial margin. The Sacrospinous Ligament This is a thin triangular ligament that
extends from the lateral margin of the sacrum and coccyx to the ischial spine. It is related anteriorly to the coccygeus muscle. The Sacroiliac Ligaments There were covered in Medicine 1
(ANAT1006). Click here to go to the sacroiliac ligaments. Back to top Joints of the Pelvis The Lumbosacral Joints L5 and S1 vertebrae articulate with each other at an anterior intervertebral joint formed by the intervertebral disc between their bodies, and at 2 posterior synovial joints between their articular processes. The L5/S1 intervertebral disc is wedge- shaped because it is thicker anteriorly. The zygapophyseal (facet) joints are synovial joints between the articular processes (inferior ones of L5 and superior ones of S1) of the two
vertebrae. The S1 facets face posteriorly and medially, thereby preventing L5 vertebrae from sliding anteriorly. L5 vertebra is also attached to the ilium
and sacrum by the strong iliolumbar ligaments. The Sacrococcygeal Joint This joint is a secondary cartilaginous joint in which fibrocartilage and ligaments join the articulating bones, the apex of the sacrum and the base of the coccyx. They are united by a thin, fibrocartilaginous intervertebral disc. The sacrococcygeal ligaments correspond to the anterior and posterior longitudinal ligaments or the other intervertebral joints. The sacral and coccygeal cornua (L. horns)
are also united by intercornual ligaments. Until middle age, there is slight
movement of the coccyx during
defecation, and considerable movement
during childbirth. In elderly persons the sacrococcygeal
joint usually becomes ossified and is
obliterated. The Sacroiliac Joints This was covered in Medicine 1
(ANAT1006). Click here to go to the sacroiliac joints. The Pubic Symphysis This was covered in Medicine 1
(ANAT1006). Click here to go to the pubic symphysis. Back to top Walls of the Pelvis The Anterior Pelvic Wall This is formed on each side by (1) the bodies of the pubic bones, and its superior and inferior rami, and (2) the obturator internus muscle and its fascia. The pubic symphysis also forms an important part of the anterior pelvic wall. The Lateral Pelvic Walls The obturator internus muscle cover most of these walls. Their superior parts, near the pelvic brim, are covered by pelvic fascia. Medial to the obturator internus on each side are the obturator nerve and vessels and other branches of the internal iliac artery. The obturator internus passes from the pelvis through the lesser sciatic foramen, and its fibres converge to form a tendon that is attached to the greater trochanter of the femur. The Posterior Pelvic Walls This wall is formed by the sacrum, adjacent parts of the ilium, and the sacroiliac joints and their ligaments. The piriformis muscles line the posterior wall laterally. These pear-shaped muscles (L. pirum, pear + forma, form) occupy a key position
in the gluteal region (buttock). Each piriformis muscle leaves the pelvis minor through the greater sciatic foramen. Medial to the piriformis muscles are the sacral plexus and the internal iliac vessels and their subsidiaries. Back to top The Floor of the Pelvis This is formed mainly by the funnel- shaped pelvic diaphragm, which is composed of the two levator ani and the two coccygeus muscles. This diaphragm closes the inferior pelvic aperture (pelvic outlet), except for a gap in the pelvic floor between the anterior edges of the levator ani muscles. This gap is filled with loose fascia around the prostate (or vagina) and is closed by the urogenital diaphragm and its superior fascia. The pelvic diaphragm also separates the pelvic cavity from the perineum. The musculofascial pelvic diaphragm supports the abdominopelvic viscera. It is slung somewhat like a funnel- shaped hammock between the pubis anteriorly and the coccyx posteriorly. Laterally, it is attached to a thickening of the obturator fascia known as the tendinous arch. The rectum and urethra, and the vagina in women, penetrate the pelvic
diaphragm to reach the exterior. The Levator Ani Muscles These are the largest and most important muscles in the pelvic floor. Posterior to them are the coccygeus muscles, which form the smaller part of the floor. The thin, broad levator ani muscles unite
with its partner to form a hammock-like
sheet of muscle between the pubis
anteriorly and the coccyx posteriorly, and
from one lateral pelvic wall to the other. The levator ani muscles form most of the
floor of the pelvic cavity, which
separates it from the wedge-shaped spaces known as the ischioanal (ischiorectal) fossae. The levator ani muscle is divided into 3 principal parts: the puborectalis, pubococcygeus, and iliococcygeus. The Puborectalis Muscle This arises from the pubis and passes posteriorly, where it unites with its partner to from a U-shaped muscular sling around the anorectal junction. This sling maintains the anorectal flexure. Some fibres of the puborectalis sweep
around the prostate in males and the middle of the vagina in females and are inserted into the central perineal ligament or tendon, or perineal body. This is a fibromuscular mass anterior to the anus. These muscle fibres constitute the levator prostatae and pubovaginalis respectively. The Pubococcygeus Muscle This is the main part of the levator ani. It arises from the pubis and runs posteromedially to insert into the coccyx and anococcygeal ligament. The anococcygeal ligament is the median fibrous intersection of the pubococcygeus muscles. It is located between the anal canal and the tip of the coccyx. The pubococcygeus muscle, as it courses inferiorly and medially, encircles the urethra, vagina, and anus and merges into the perineal body. The Iliococcygeus Muscle This is the thin part of the levator ani. It arises on each side from the tendinous arch of the obturator fascia and the ischial spine. Each muscle passes medially and posteriorly and attaches to the coccyx and anococcygeal ligament. Innervation of the Levator Ani Muscles They are innervated by the perineal branches of the 3rd and 4th sacral nerves, which enter its pelvic surface. Actions of the Levator Ani Muscles As the pelvic diaphragm it resists the downward thrust associated with an increase of intra-abdominal pressure (e.g., coughing). Acting together, the levator ani muscles raise the pelvic floor, thereby assisting the anterior abdominal muscles in compressing the abdominal and pelvic
contents. This action is important part of forced
expiration, coughing, vomiting,
micturition, and fixation of the trunk
during strong movements of the upper
limbs. The parts of the levator ani muscles that
insert into the perineal body (tendinous centre of the perineum) support the prostate (levator prostatae) in males. In females, these parts support the
posterior wall of the vagina
(pubovaginalis). The parts of the levator ani muscles that
insert into the wall of the anal canal holds the anorectal junction anteriorly, thereby increasing the angle between the rectum and anal canal. This prevents the passage of faeces
between the rectum and anal canal when defecation is not desired or is
inconvenient. When these parts contract, they raise the canal over a descending mass of faeces, thereby aiding defecation. During parturition, the levator ani muscles support the foetal head, while the cervix of the uterus is dilating. Back to top The Coccygeus Muscles This is a triangular sheet of muscle that lies against the posterior part of the iliococcygeus muscle with which it is continuous. These along with the levator ani muscle form the pelvic diaphragm. The coccygei form the posterior and smaller part of the pelvic floor, which is formed by the pelvic diaphragm. Lateral attachment: pelvic surfaces of ischial spine and sacrospinous ligament. Medial attachment: lateral margin of the coccyx and S5 vertebra. Innervation: branches of S4 and S5 nerves. The coccygeus muscles assist the levator ani muscles in supporting pelvic viscera. They also support the coccyx and pull it anteriorly, elevating the pelvic floor.
Subscribe to:
Post Comments (Atom)

No comments:
Post a Comment