Urogenital Diaphragm and
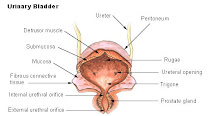
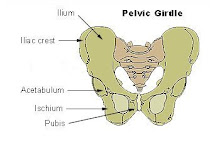
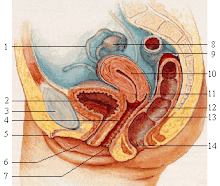
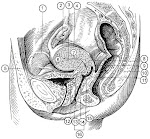
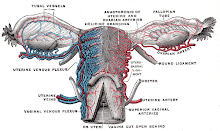
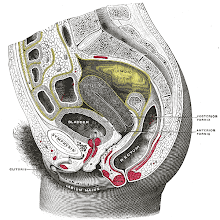
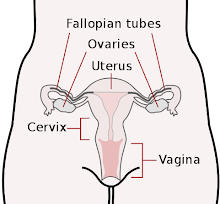
Ischiorectal Fossa The Urogenital Diaphragm This is a thin sheet of striated muscle stretching between the two sides of the pubic arch. It covers the anterior part of the inferior pelvic aperture (pelvic outlet). The most anterior and posterior fibres of the urogenital diaphragm (deep transverse perineal muscle) run transversely. The middle fibres (sphincter urethrae muscle) surround the membranous urethra. Sphincter Urethrae Muscle This muscle is attached to the medial surface of the inferior pubic ramus. Its fibres pass medially toward the urethra, where they meet the fibres from the opposite side. Some fibres encircle the membranous urethra in the male and form a true voluntary sphincter that compresses the urethra. It also extends to the base of the bladder and invests the prostate anteriorly and anterolaterally. In the female, the inferior 1/2 of the sphincter urethrae blends with the anterolateral walls of the vagina, forming a urethrovaginal sphincter that compresses the urethra and vagina. Innervation: perineal nerve, a branch of the pudendal nerve (S2, S3 and S4). This voluntary sphincter of the urethra constricts the membranous urethra in the male and compresses the urethra and vagina in the female. Deep Transverse Perineal (Transversus
Perinei) Muscle This is a narrow slip of muscle that is attached to the medial surface of the ischial ramus. It runs transversely to insert into the perineal body (central perineal tendon). In the female, some fibres also insert into the vaginal wall. Innervation: perineal nerve, a branch of the pudendal nerve (S2, S3 and S4). This muscle steadies the perineal body, thereby contributing to the general supportive role of the urogenital diaphragm for the pelvic floor and viscera. The Perineal Body The tendinous centre of the perineum or perineal body is a small wedge-shaped mass of fibrous tissue located at the centre of the perineum. The perineal body is the landmark of the perineum, where several muscles converge: the transverse perineal, bulbospongiosus, levator ani and some fibres of the external anal sphincter. Back to top The Perineal Fascia The urogenital diaphragm is surrounded
by deep fascia. The perineal fascia consists of two sheets, the inferior and superior fasciae of the urogenital diaphragm. The Inferior Fascia of Urogenital
Diaphragm This is usually referred to as the perineal membrane. It is continuous with the superior fascia of the urogenital diaphragm. It is also attached to the pubic rami. The Superior Fascia of the Urogenital
Diaphragm The membranous layer of the subcutaneous connective tissue of the perineum (Colles' fascia) and inferior part anterior abdominal wall are continuous. The attachments of the superior perineal fascia are: 1. The fascia lata enveloping the thigh muscles; 2. The pubic arch; 3. And the posterior edge of the perineal membrane. Anteriorly, the superficial perineal fascia
is prolonged over the penis and scrotum, thereby forming a membranous covering for the testes and spermatic cords (in males). In the female, this fascia is prolonged over the clitoris and labia majora. Back to top The Superficial Perineal Space This is the space between the superficial perineal fascia and the perineal membrane. The superficial perineal fascia attaches
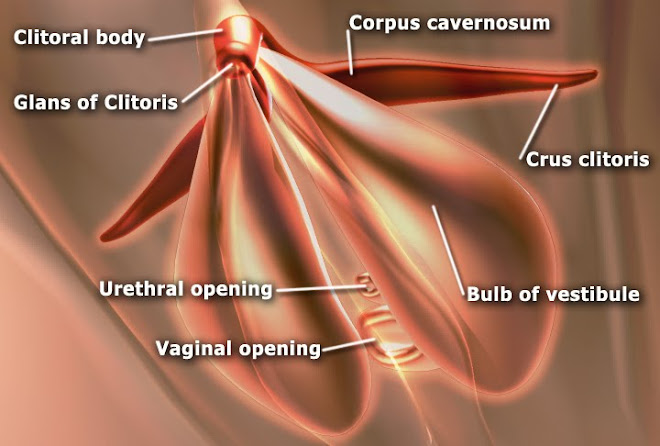
medially to the superior border of the pubic symphysis and laterally to the body of the pubis. Contents of the Superficial Perineal Space In the male, this space contains: 1. The root of the penis and the muscles associated with it; 2. The contents of the scrotum; 3. The proximal part of the spongy urethra; 4. The superficial perineal muscles; 5. The branches of the internal pudendal vessels; 6. And the pudendal nerves. In the female, this space contains: 1. The root of the clitoris; 2. The bulbs of the vestibule; 3. The superficial perineal muscles; 4. The related vessels and nerves; 5. And the great vestibular glands. Back to top The Deep Perineal Space This is the fascial space enclosed by the superior and inferior fasciae of the urogenital diaphragm. The two layers of fascia are attached
laterally to the pubic arch and blend with each other anteriorly at the apex and posteriorly at the base of the urogenital diaphragm. The deep dorsal vein of the penis enters the pelvis between its anterior edges
(transverse perineal ligament) and the arcuate pubic ligament. Contents of the Deep Perineal Space In the male, the deep perineal space contains: 1. The membranous urethra; 2. The sphincter urethrae muscle; 3. The bulbourethral glands; 4. The deep transverse perineal muscles; 5. And related vessels and nerves. In the female, the deep perineal space contains: 1. Part of the urethra; 2. The sphincter urethrae muscles; 3. The deep transverse perineal muscle; 4. And related vessels and nerves. Back to top The Ischiorectal (ischioanal)
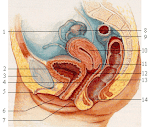
Fossae This is a large, fascia-lined, wedge- shaped space on each side of the rectum or anal canal. It is located between the skin of the anal region and the pelvic diaphragm. The apex of each ischiorectal fossa lies superiorly, at the point where the levator ani muscle arises from the obturator fascia. The apex of each fossa is located about 6 cm superior to the ischial tuberosity. The base of each fossa is formed by perianal skin. Because the two levator ani muscles are shaped like a funnel, the ischiorectal
fossae are wide inferiorly and narrow superiorly. Anteriorly, the ischiorectal fossae
continue superior to the urogenital diaphragm, where they form the anterior recesses of the ischiorectal fossae. These spaces are filled with loose
connective tissue. There are also posterior recesses where the gluteus maximus muscle overhangs the ischiorectal fossa. The 2 ischiorectal fossae communicate over the anococcygeal ligament. Posteriorly, each fossa is also continuous
with the lesser sciatic foramen, superior to the sacrotuberous ligament. Boundaries of the Ischiorectal Fossae Each fossa is bounded: Laterally: the ischium and the inferior part of the obturator internus muscle. Medially: the anal canal to which the levator ani and external anal sphincter are applied. Posteriorly: the sacrotuberous ligament and gluteus maximus muscle Anteriorly: the base of the urogenital diaphragm and its fasciae. Contents of the Ischiorectal Fossae These wedge-shaped fascial spaces are
filled with soft fat, called the ischiorectal pads of fat. They are traversed by many tough, fibrous bands and septa. These fibrofatty pads support the anal canal, but they can be readily displaced to permit the anal canal to expand when faeces are present. The ischiorectal fossae also contain the internal pudendal artery and vein and the pudendal nerve. These structures run on the lateral walls of the fossae in the fibrous canals called the pudendal canals. Posteriorly, these vessels and the
pudendal nerve give off the inferior rectal vessels and nerves. These structures become superficial as
they pass toward the surface to supply the external anal sphincter and the perianal skin. Two other cutaneous nerves, the perforating branch of S2 and S3 nerves and the perineal branch of S4 nerve also pass through the ischiorectal fossae.
Subscribe to:
Post Comments (Atom)

No comments:
Post a Comment